Last Updated on March 22, 2023 by admin
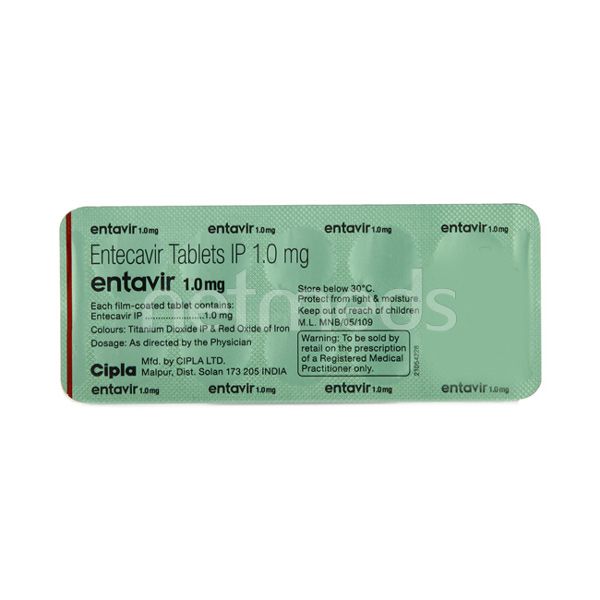
Entavir 1mg Tablet
Entavir 1mg – Overview
INTRODUCTION
Entavir 1mg Tablet is used in the treatment of HIV infection and chronic hepatitis B virus (HBV) infection. It prevents the multiplication of virus in human cells. This stops the virus from producing new viruses and clears up your infection.
Entavir 1mg Tablet is not a cure for HIV or AIDS and only helps to decrease the amount of HIV in your body. This helps to lower your risk of getting HIV-related complications and improves your lifespan. It is prescribed in combination with other HIV medicines. Your doctor will recommend the best medicines for you and will decide the doses that you need. Follow carefully the instructions for all the medicines that you are given. It can be taken with or without food. Taking all these medicines regularly at the right times greatly increases their effectiveness and reduces the chances of HIV becoming resistant to them. It is important not to miss doses and to keep taking them until your doctor tells you it is safe to stop.
Common side effects of this medicine include headache, nausea, vomiting, stomach pain, fatigue, diarrhea, and rash. These are usually not serious but tell your doctor if they bother you or do not go away. Rarely, some people may experience a skin reaction or liver damage. Your doctor will closely monitor you for these in the initial period of treatment.
Before taking it, tell your doctor if you have any skin problems or liver or kidney disease. While using it, you may need regular blood tests to check your blood counts and liver function. Avoid drinking alcohol as it may increase your risk of liver damage. Pregnant or breastfeeding mothers should consult their doctor before using this medicine. Do not have unprotected sex or share personal items like razors or toothbrushes, if you are HIV positive. Talk to your doctor about safe ways like condoms to prevent HIV transmission during sex.
USES OF ENTAVIR TABLET
- Chronic hepatitis B virus (HBV) infection
BENEFITS OF ENTAVIR TABLET
- In Chronic hepatitis B virus (HBV) infection
In patients with chronic hepatitis B virus (HBV) infection, Entavir 1mg Tablet works by preventing the HBV virus from multiplying in the body. It helps control the infection and makes the immune system work better. This lowers the chances of getting complications and improves the quality of life.
This medicine is always taken in combination with other antiretroviral medicines. It is not a cure and should neither be used to prevent HBV infection. It is important that you take this medicine as prescribed, following the dosage recommended by your doctor. Taking all doses in the right amount at the right times greatly increases the effectiveness of the medicine.
SIDE EFFECTS OF ENTAVIR TABLET
Most side effects do not require any medical attention and disappear as your body adjusts to the medicine. Consult your doctor if they persist or if you’re worried about them
Common side effects of Entavir
- Headache
- Nausea
- Rash
- Vomiting
- Fatigue
- Stomach pain
- Diarrhea
HOW TO USE ENTAVIR TABLET
Take this medicine in the dose and duration as advised by your doctor. Swallow it as a whole. Do not chew, crush or break it. Entavir 1mg Tablet is to be taken empty stomach.
HOW ENTAVIR TABLET WORKS
Entavir 1mg Tablet is an antiviral medication. It prevents the multiplication of virus in human cells. This stops the virus from producing new viruses and clears up your infection.
SAFETY ADVICE
warnings
![]() Alcohol
Alcohol
CONSULT YOUR DOCTOR
It is not known whether it is safe to consume alcohol with Entavir 1mg Tablet. Please consult your doctor.
warnings
![]() Pregnancy
Pregnancy
CONSULT YOUR DOCTOR
Entavir 1mg Tablet may be unsafe to use during pregnancy. Although there are limited studies in humans, animal studies have shown harmful effects on the developing baby. Your doctor will weigh the benefits and any potential risks before prescribing it to you. Please consult your doctor.
warnings
![]() Breast feeding
Breast feeding
CONSULT YOUR DOCTOR
Entavir 1mg Tablet is probably unsafe to use during breastfeeding. Limited human data suggests that the drug may pass into the breastmilk and harm the baby.
warnings
![]() Driving
Driving
UNSAFE
Entavir 1mg Tablet may decrease alertness, affect your vision or make you feel sleepy and dizzy. Do not drive if these symptoms occur.
warnings
![]() Kidney
Kidney
CAUTION
Entavir 1mg Tablet should be used with caution in patients with kidney disease. Dose adjustment of Entavir 1mg Tablet may be needed. Please consult your doctor.
warnings
![]() Liver
Liver
SAFE IF PRESCRIBED
Entavir 1mg Tablet is safe to use in patients with liver disease. No dose adjustment of Entavir 1mg Tablet is recommended.
warnings
![]() CHILDREN CAUTION
CHILDREN CAUTION
UNSAFE
Entavir 1mg Tablet is not recommended for use in children and adolescents below 18 years.
![]() Entavir 1mg Tablet Habit Forming : NO
Entavir 1mg Tablet Habit Forming : NO
![]() expert advice
expert advice
WHAT IF YOU FORGET TO TAKE ENTAVIR TABLET?
If you miss a dose of Entavir 1mg Tablet, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular schedule. Do not double the dose.
- You have been prescribed Entavir 1mg Tablet for the treatment of chronic hepatitis B virus (HBV) infection.
- Take it on an empty stomach, at least 2 hours after or before a meal.
- Entavir 1mg Tablet may cause dizziness or sleepiness. Do not drive or do anything requiring concentration until you know how it affects you.
- You may still develop infections or other illnesses associated with viral infection while taking this medication.
- During treatment and for at least six months after stopping this medicine, regular blood tests are needed to monitor your liver function, level of hepatitis B virus and blood cells in your blood.






















There are no reviews yet.