Understanding Mantle Cell Lymphoma: A Step-by-Step Guide
Introduction to Mantle Cell Lymphoma
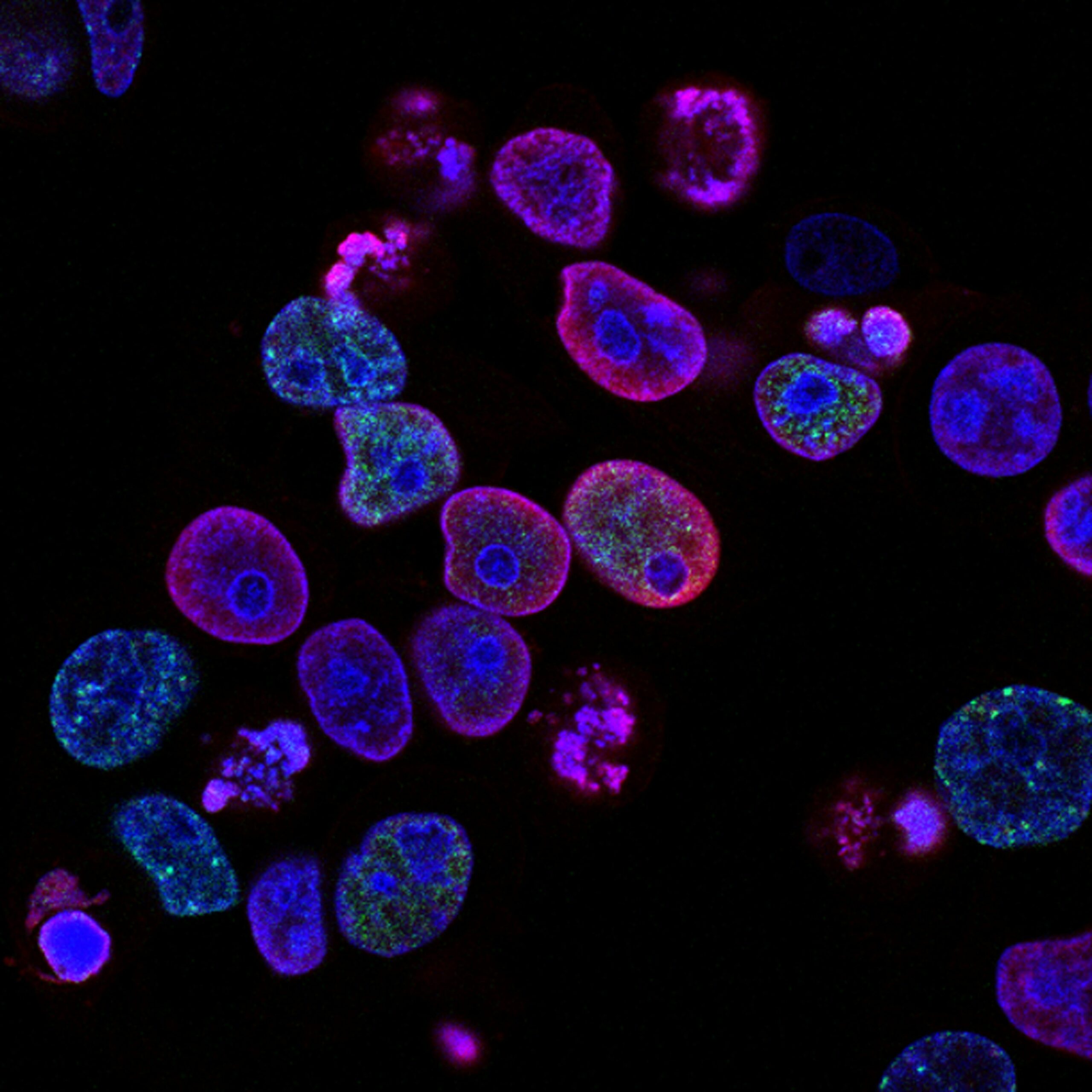
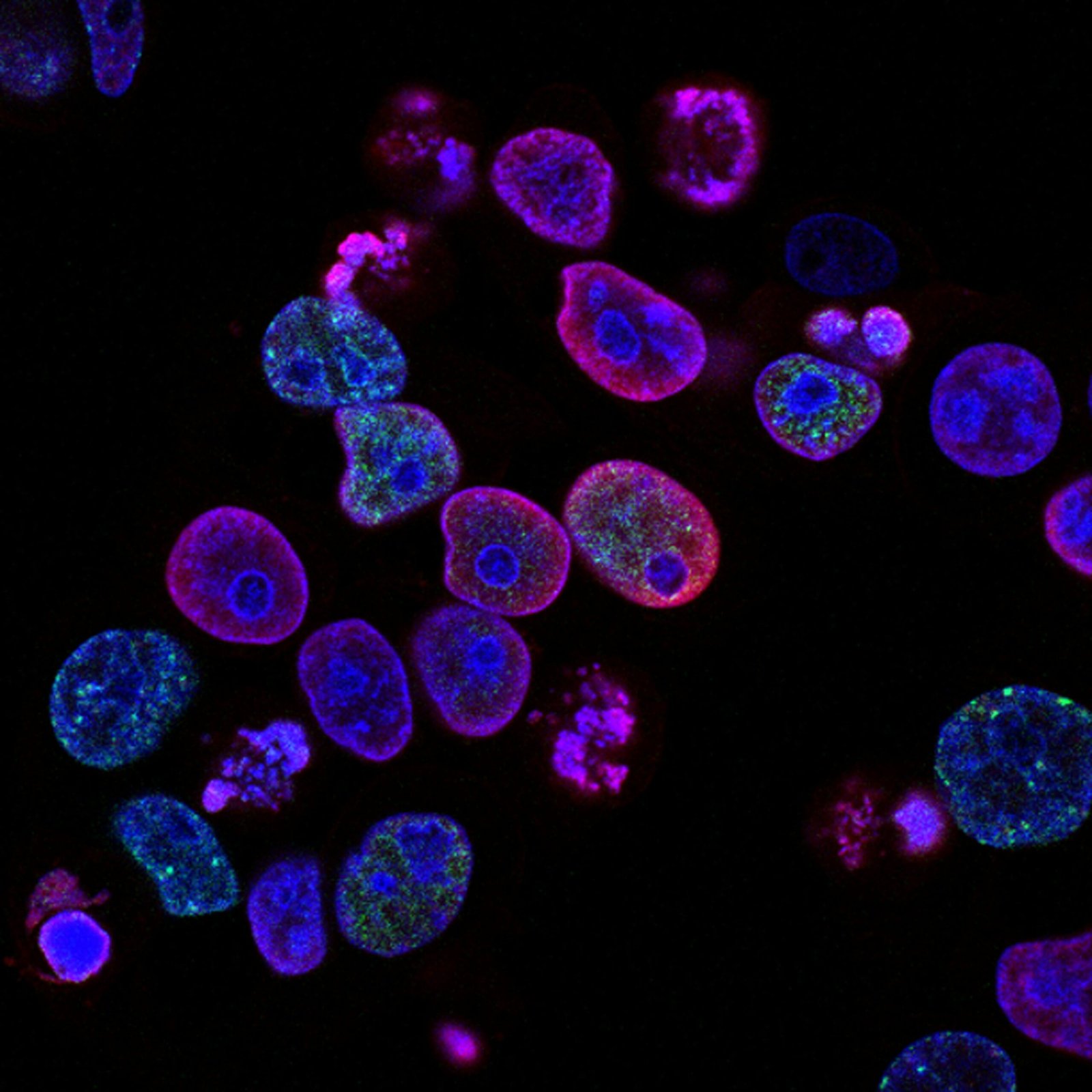
Mantle Cell Lymphoma (MCL) is a relatively rare form of non-Hodgkin lymphoma, accounting for approximately 6% of all non-Hodgkin lymphoma cases. This type of lymphoma originates from B cells, a type of white blood cell that plays a crucial role in the immune system by producing antibodies to fight infections. MCL is characterized by the abnormal growth of cancerous B cells in the mantle zone, an area surrounding the lymph node follicles. This uncontrolled proliferation leads to the formation of tumors in the lymph nodes and can spread to other parts of the body, including the bone marrow, spleen, and gastrointestinal tract.
The significance of early diagnosis in MCL cannot be overstated. Due to its aggressive nature and tendency to spread rapidly, timely identification and treatment are critical for improving patient outcomes. Symptoms of MCL can be non-specific and may include swollen lymph nodes, fatigue, fever, night sweats, and unexplained weight loss. These symptoms can easily be mistaken for other, less severe illnesses, which underscores the importance of awareness and prompt medical consultation if such symptoms persist.
MCL was first described in the 1970s, and its classification has evolved over the years as our understanding of the disease has deepened. Initial research identified it as a distinct subtype of non-Hodgkin lymphoma, and subsequent studies have provided insight into its genetic and molecular underpinnings. Notably, the overexpression of cyclin D1, a protein that regulates cell cycle progression, is a hallmark of MCL and serves as a key diagnostic marker.
For more detailed information on Mantle Cell Lymphoma, reputable sources such as the Mayo Clinic and the American Cancer Society offer comprehensive guides and updates on ongoing research. Their contributions to the field have been instrumental in improving diagnostic techniques and developing targeted therapies that offer hope to those affected by this challenging disease.
Causes and Risk Factors
Mantle Cell Lymphoma (MCL) is a form of non-Hodgkin lymphoma that is characterized by the malignant transformation of B-cells. One of the primary genetic anomalies associated with MCL is a translocation between chromosomes 11 and 14. This translocation results in the overexpression of the cyclin D1 gene, which plays a crucial role in cell cycle regulation. The aberrant activation of this gene leads to uncontrolled cellular proliferation, a hallmark of cancerous growth.
While the exact causes of Mantle Cell Lymphoma are not entirely understood, several risk factors have been identified. Age is a significant risk factor, as MCL is most commonly diagnosed in individuals over the age of 60. Gender also plays a role; men are more frequently affected by MCL compared to women. Family history is another contributing factor, with individuals having a close relative with lymphoma or other cancers being at a higher risk.
Aside from genetic predispositions, environmental factors and lifestyle choices do not appear to have a significant impact on the development of MCL. However, ongoing research continues to explore potential links between environmental exposures and the onset of this disease.
For those seeking more detailed information on the genetic and molecular mechanisms driving Mantle Cell Lymphoma, as well as comprehensive risk assessments, several reputable sources are available. The Leukemia & Lymphoma Society provides extensive resources and up-to-date research findings. Additionally, academic journals and research articles, accessible through platforms such as PubMed, offer in-depth analyses and studies on the genetic mutations and risk factors associated with MCL.
Mantle cell lymphoma (MCL) presents with a range of symptoms that can often be mistaken for other illnesses, making early diagnosis challenging. Among the most common symptoms are swollen lymph nodes. These enlargements, which may initially be painless, can occur in various parts of the body, including the neck, armpit, and groin.
Patients with MCL often experience systemic symptoms such as fever, night sweats, and unexplained weight loss. These symptoms, known collectively as “B symptoms,” are indicative of an active disease process. Night sweats are typically drenching and can interfere significantly with sleep quality, while the unexplained weight loss can be rapid and severe, affecting overall health and wellbeing.
The variability in symptoms is noteworthy. For instance, John, a 52-year-old MCL patient, reported only mild fatigue and occasional fevers before his diagnosis. In contrast, Maria, a 60-year-old, experienced persistent night sweats and significant weight loss, leading to an earlier identification of her condition. Such patient testimonials underscore the wide range of experiences and highlight the importance of considering MCL in differential diagnoses.
Other less common symptoms might include gastrointestinal issues, such as nausea and bloating, which arise if lymphoma cells infiltrate the digestive tract. Additionally, some patients might experience anemia, leading to feelings of weakness and breathlessness.
Given the overlap of MCL symptoms with those of more common illnesses, it is crucial for individuals experiencing persistent or unexplained symptoms to seek medical evaluation. For more detailed descriptions of MCL symptoms, the National Cancer Institute provides comprehensive resources. Understanding these symptoms can facilitate earlier detection and improve treatment outcomes for those affected by mantle cell lymphoma.
Diagnosis and Staging
Mantle Cell Lymphoma (MCL) diagnosis typically begins with a comprehensive physical examination, where a healthcare provider assesses for swollen lymph nodes, spleen, or liver. If MCL is suspected, a biopsy is often the next step. A tissue sample is taken from the lymph node or another suspicious area and analyzed under a microscope to identify the characteristic features of MCL.
In addition to biopsies, various imaging tests are crucial for diagnosing and staging MCL. Computed Tomography (CT) scans and Positron Emission Tomography (PET) scans are commonly used. These imaging techniques provide detailed pictures of the inside of the body, helping to locate lymphoma and determine its extent.
Blood tests are also essential in the diagnostic process. Full blood counts and lactate dehydrogenase (LDH) levels can offer valuable information. Additionally, flow cytometry and immunophenotyping are specialized tests that analyze the characteristics of lymphoma cells, confirming the diagnosis of MCL.
The staging of Mantle Cell Lymphoma is a critical step in treatment planning. The staging process assesses the spread of the lymphoma within the body. MCL is typically staged using the Ann Arbor staging system, which ranges from Stage I (limited to one lymph node region) to Stage IV (spread to distant organs like the bone marrow or liver).
Specific diagnostic criteria for MCL include the detection of cyclin D1 overexpression or the presence of the t(11;14) translocation, which are hallmarks of the disease. Oncologists use these criteria, along with clinical and imaging findings, to confirm the diagnosis and stage the lymphoma accurately.
For more detailed information on the diagnosis and staging of Mantle Cell Lymphoma, resources from the American Society of Hematology and other reputable medical institutions provide comprehensive guidelines and updates on best practices.
Treatment Options
Mantle Cell Lymphoma (MCL) presents a range of treatment options, each selected based on the specific stage and aggressiveness of the disease. Chemotherapy remains a cornerstone treatment, often used in combination with other modalities. It employs potent drugs to kill cancer cells, but it also affects healthy cells, leading to side effects such as fatigue, nausea, and increased susceptibility to infections. Despite these drawbacks, chemotherapy can be highly effective in reducing tumor size and achieving remission in patients with MCL.
Targeted therapy represents a more modern approach, focusing on specific molecules involved in cancer cell growth and survival. Drugs like ibrutinib and acalabrutinib inhibit enzymes critical for MCL cell proliferation. These therapies generally result in fewer side effects compared to traditional chemotherapy, although they can still cause issues such as bleeding and heart problems. Targeted therapies are particularly beneficial for patients with relapsed or refractory MCL.
Immunotherapy harnesses the body’s immune system to fight cancer. Monoclonal antibodies, such as rituximab, attach to cancer cells and mark them for destruction by the immune system. This method can be effective and is often combined with chemotherapy. However, side effects like infusion reactions and flu-like symptoms may occur. Recent advancements include CAR T-cell therapy, an innovative treatment where a patient’s T-cells are engineered to attack cancer cells, showing promising results in clinical trials.
Stem cell transplants offer another treatment avenue, particularly for younger patients or those in good health. High-dose chemotherapy is followed by the infusion of stem cells to restore the bone marrow. While this method can lead to long-term remission, it carries significant risks including infections and organ damage.
Recent advancements and clinical trials continue to refine these treatment strategies. The National Comprehensive Cancer Network (NCCN) and other authoritative sources provide up-to-date guidelines and recommendations, ensuring that patients receive the best possible care based on the latest scientific evidence.
Managing Side Effects and Complications
Mantle Cell Lymphoma (MCL) treatments, while critical for combating the disease, often come with a range of side effects and complications that can significantly impact patients’ quality of life. Understanding these challenges and adopting effective management strategies is essential for maintaining well-being during treatment.
One of the most common side effects of MCL treatments is nausea. This can be distressing and may reduce a patient’s ability to maintain proper nutrition. Anti-nausea medications, prescribed by doctors, can be quite effective. Additionally, small, frequent meals and avoiding spicy or greasy foods can help manage symptoms. Ginger tea and acupressure wristbands are also often recommended as complementary approaches.
Fatigue is another pervasive issue for MCL patients undergoing treatment. It is crucial to balance activity with rest, as overexertion can exacerbate tiredness. Patients should prioritize tasks, delegate when possible, and incorporate short naps into their day. Gentle exercises like walking or yoga can also boost energy levels and improve overall stamina.
Infection risk is elevated in MCL patients due to weakened immune systems from both the disease and its treatments. Practicing good hygiene, such as frequent handwashing and avoiding contact with sick individuals, is vital. Patients may also need to adhere to specific dietary restrictions to avoid foodborne illnesses. Regular monitoring by healthcare providers ensures early detection and prompt treatment of any infections that arise.
Lifestyle changes play a crucial role in managing side effects and enhancing quality of life. A balanced diet rich in fruits, vegetables, and lean proteins supports overall health. Staying hydrated and getting adequate sleep are equally important. Psychological support, through counseling or support groups, helps manage the emotional toll of the disease. Organizations like CancerCare and the Lymphoma Research Foundation offer valuable resources, including patient education, support groups, and financial assistance.
By adopting these strategies and utilizing available resources, MCL patients can better navigate the complexities of their treatment journey, mitigating side effects, and maintaining a higher quality of life.
Living with Mantle Cell Lymphoma
Mantle cell lymphoma (MCL) poses unique challenges for long-term survivorship, requiring a comprehensive approach that addresses both physical and mental health needs. Living with MCL often involves navigating a complex journey of treatments, follow-up care, and the constant vigilance needed to monitor for recurrence.
Long-term survivorship issues can include managing the side effects of treatments such as chemotherapy and radiation, which may affect overall health and quality of life. Patients may experience fatigue, cognitive changes, or cardiovascular issues, necessitating a multidisciplinary approach for optimal care. Regular follow-up appointments are crucial, as they allow for early detection of any signs of recurrence and timely intervention.
Mental health is another critical aspect of living with MCL. The emotional toll of a cancer diagnosis and the ongoing uncertainty can lead to anxiety, depression, and stress. It is essential for patients to have access to mental health support services, including counseling and support groups, to help manage these challenges. Sharing stories of individuals who have successfully managed their condition can provide hope and encouragement. For instance, John, a 55-year-old MCL survivor, emphasizes the importance of a positive mindset and staying informed about his condition. By actively participating in his treatment plan and seeking support, he has been able to maintain a good quality of life.
Access to survivorship resources can significantly enhance the journey of living with MCL. Organizations such as the Leukemia & Lymphoma Society offer comprehensive support services, including educational materials, peer support networks, and financial assistance. Additionally, mental health resources such as the Cancer Support Community provide invaluable support for emotional well-being.
In conclusion, living with mantle cell lymphoma requires a holistic approach that integrates regular follow-up care, mental health support, and access to survivorship resources. By addressing these aspects, patients can navigate their journey with MCL more effectively, improving their overall quality of life.
Future Directions in Mantle Cell Lymphoma Research
The landscape of Mantle Cell Lymphoma (MCL) research is rapidly evolving, offering hope for more effective treatments and better patient outcomes. One of the most promising avenues is the development of personalized medicine. By leveraging advances in genetic research, scientists aim to tailor therapies based on the unique genetic profile of each patient’s cancer. This approach not only enhances treatment efficacy but also minimizes adverse effects.
Recent studies have identified several genetic mutations associated with MCL, paving the way for targeted therapies. For instance, inhibitors targeting the Bruton’s tyrosine kinase (BTK) gene, such as Ibrutinib, have shown significant promise. Ongoing clinical trials are exploring the efficacy of combining these targeted treatments with traditional chemotherapy and immunotherapy, potentially revolutionizing the standard care protocols.
Research institutions like the American Association for Cancer Research and the National Cancer Institute are at the forefront of these advancements. These organizations are funding and conducting numerous studies aimed at understanding the molecular mechanisms driving MCL. Their contributions are invaluable in identifying novel biomarkers for early detection and monitoring disease progression.
The role of immunotherapy in MCL treatment is another exciting area of research. Therapies such as CAR-T cell therapy, which involves genetically modifying a patient’s own T cells to attack cancer cells, are currently under investigation. Preliminary results from clinical trials are promising, showing potential for long-term remission in certain patients.
For those interested in keeping abreast of the latest findings, scientific journals like Blood and the Journal of Clinical Oncology regularly publish significant research on MCL. These publications offer in-depth insights into ongoing studies and emerging therapies.
In summary, the future of Mantle Cell Lymphoma research is bright, with numerous innovative treatments on the horizon. The integration of personalized medicine, genetic research, and advanced immunotherapies holds the potential to transform the treatment landscape, offering new hope to patients worldwide.